I am advising on Blockchain/Distributed Ledger Technology (DLT) for the Grapevine Healthcare project.
This article discusses the issue of interoperability and blockchain in the healthcare domain.
There article is organised into two parts:
- The first part explains how the Healthcare Information Technology industry could achieve a good level of interoperability.
- The second part exposes what I consider some common pitfalls affecting a number of blockchain use-cases that were brought to my attention while attending some DLT-related events.
The introduction of IT systems in the healthcare domain began in the 80s, with the advent of initiatives such as DICOM, and Health Level 7 which made the first steps towards digitalisation.
The ISO 27002 specification defines the guidelines for IT system security regarding CIA triad, Confidentiality, Integrity, and Availability.
Availability in particular ensures that authorised users have access to information and associated assets when required.
We're in an emergency room of a hospital. A patient arrives unconscious and the doctor needs to decide whether or not to treat him with a specific antibiotic.
The doctor doesn't know anything about the pre-existing medical conditions of the patient—like potential allergies—so she searches the hospital's local IT system for ther patient's medical records (remember, since the 90s electronic medical records have been available and in some parts of the world they only exist in digital format).
The emergency room client software uses HL7v3 and tries to access the central clinical document repository, which—by contrast—only understands HL7 FHIR.
No interoperability is possible between the HL7v3 client system and the FHIR repository system. The lack or architecture is evident, and this is likely to lead to vendor lock-in.
The patient's safety is at risk, since the medical records are not available.
Now, let's look at the issue in a global scale scenario. Let's say, for example, that the patient is in a foreign country travelling, and the doctor needs to fetch medical records from the patient's home country.
Can you evaluate the risk of not having interoperability?
Here are some elements to consider:
- language barriers
- medical disciplines
- medicine types
- dosage variance
- electronic message types
- security models
This is a scenario where a properly designed IT software architecture would help.
The case for interoperability is compelling, but how do we achieve it?
[Bass et al.] identify interoperability as the degree to which two or more systems can usefully exchange meaningful information via interfaces in a particular context. A world working on a unique software infrastructure is a not a realistic scenario (see Section on EIF); thus different vendors around the globe must agree on common rules for interoperability, but to which extent?
Here is how HiMMS, the most prominent worldwide healthcare IT society, defines interoperability:
In healthcare, interoperability is the ability of different information technology systems and software applications to communicate, exchange data, and use the information that has been exchanged. Data exchange schema and standards should permit data to be shared across clinician, lab, hospital, pharmacy, and patient regardless of the application or application vendor.
There are three levels of health information technology interoperability:
- Foundational (at the level of message exchange),
- Structural (the format of data exchange),
- Semantical (at the level of the information exchanged).
The EU EIF, the ISA European Interoperability Reference Architecture, and the e-SENS project introduced 2 more interoperability levels as shown in the picture below:
The HiMMS definition covers only data exchange (second level), while e-SENS has added both organisational and legal interoperability to the mix, because cross country interoperability is one of the aim of the project.
Vendors shall apply to common rules. Those rules are set by international standards. Still, Grace Lewis ([Bass et al.]) explicitly mentions that "standards alone are not enough to guarantee interoperability".
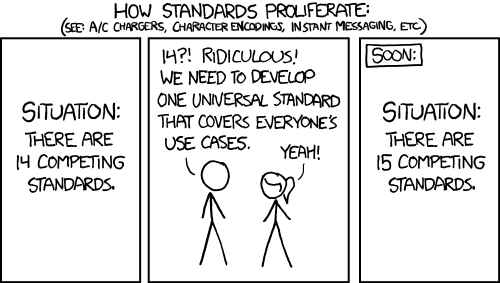
Andy Tanembaum once said "The nice thing about standards is that you have so many to choose from" which is undoubtedly true.
Standards, without any governance, cannot really achieve interoperability. Anyone can introduce a standard! But in order to get it adopted it ought to be supported, implementable, testable, and free.
Enterprise Architectures come to the rescue.
In fact, another architectural step has to be adopted - precisely the establishment of a governing structure over the precise selection of standards - to ensure a continuum of the economic and technical investments, such that a chosen technology will survive beyond the vendors proposing it and the possible deviations from the original intended standards. Having a so-called Vendor Neutral Architecture (VNA) provides an example of this. These concepts feed into to the definition of enterprise architecture.
The two ground concepts in the architecture design process are the Reference Architecture and the Solution Architecture.
- A Reference Architecture is the generic architecture that provides guidelines and options for the development of specific architectures and solution implementations.
- A Solution Architecture describes the particular business operations/activities and how the information systems and technology support them. It typically applies to a single project/organisation.
Agilists may comment that architeture it's a bit of a waterfall excercise (BDUF), and might not be needed at all (YAGNI). Criticisms to this point are described in the works of [Meyer] and [Babar et al.].
TOGAF, the SGAM, and IHE provide a methdological means to define the solution and reference architectures. In particular, IHE has been regulated by the EU commission with decision [(EU) 2015/1302 of 28 July 2015](https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=OJ:JOL_2015_ 99_R_0011).
We, therefore, understand that we need interoperability to develop and choose sofwtware for healthcare. To achieve interoperability we need a standard, no, wait, we need a organisation which supports and governs the standards, then we need to test, certify, oh my! Isn't it better to all select the same prodfuct and deploy it worldwide? No. Here the story of the European Interoperability Framework (EIF) and the Free Software Foundation comes into play.
At the beginning of the century, the EU commission made the right decision: to make interoperability mandatory amongst public services in Europe. A hypothetical IT employee within the EU would have said, "We know that a standard is not sufficient, so we bring in a Enterprise Architecture framework.". EIF quickly evolved to version 2.0 which raised a substantial political debate due to political lobbying from the Business Software Association (BSA). The Free Software Foundation produced a statement as follows:
Looking back to the consultation draft, it is obvious that during the development of EIFv2, the European Commission has abandoned the concept of Open Standards as a key enabler for interoperability. This is a central reason why the current draft would see the European Interoperability Framework become a shadow of its former self.
The basic idea of the Business Software Alliance lobbying was that software homogeneity guarantees interoperability, while other approaches, well, probably not. BSA clearly wanted to achieve a vendor lock-in situation, disqualifying the continuum concept described above. The EIFv3 (or the New EIF) explicitly promotes open standards, and Free Software has been indicated as one of the factors of enhanced interoperability. This new version "focus on openness and information management, data portability, interoperability governance, and integrated service delivery." as Reported by the Commission.
Blockchain is a distributed ledger, and is, in this text from now on referred to as a Distributed Ledger Technology (DLT). [Wattenhofer] defines the blockchain as the longest path from the genesis block, i.e., root of the tree, to a leaf. The blockchain acts as a consistent transaction history on which all nodes eventually agree. On each transaction some code can be executed in different ways and takes different names (e.g., Smart Contracts, Chaincode, etc). From this definition it should be clear what a blockchain is not: an efficient database. Storing unstructured data in a blockchain guarantees poor performance but still, depends on the blockchain deployment, whether public or private and on the consensus algorithm: private blockchain can run a more efficient consensus strategy (or don't need one at all) since there is a certain level of trust amongst the nodes. [Here](https://blockchainatberkeley.blog/building-it-better-a-simple-guide-to- blockchain-use-cases-de494a8f5b60) and here there are pretty famous blockchain papers on proper DLTs use.
Some projects, like Ethereum, store data in a public blockchain. However this introduces several problems in the healthcare domain:
- Apart from storage costs, without a freely given informed consent you cannot disclose medical data
- Data in the blockchain is publicly accessible
Some projects solve 1) and 2) by using encryption, but it is unwise to trust an encryption algorithm forever. The [NIST](https://csrc.nist.gov/Projects/Cryptographic-Standards-and-Guideline s) or [ENISA](https://www.enisa.europa.eu/topics/data-protection/security-of-perso nal-data/cryptographic-protocols-and-tools) update the list of useable algorithms every five years, on average.
Some other projects rely on Smart Contracts: however this introduces another IT security problem. Ethereum, writes a smart contract, "in stone". However, at the time of writing, Solidity is at version 0.4.xx, and there are some rumors about its design flaws, and if a bug is introduced in the contract code it can't be simply corrected. Of course, smart contracts are audited, but the auditor performs static analysis checks using today's security knowledge, which can change in future, thereby introducing new issues and breaches. Moving between contracts version in Ethereum is an hard work (e.g., via the proxy call). Other DLT (such as Hyperledger) allows the update of smart contract's code. But then, if few people can update a smart contract potentially holding economic value, we inherit the IT security problem of, who is entitled to change the contract? We loose the benefit of cryptography (the immutability of the smart contract), by rephrasing it as an IT Security problem (IA&A). Moreover, most of the auditors that I encountered, do not disclose the real persons behind the audit, and usually, audits are performed by creating some unit (e.g., with Truffle) tests, which is basically only defining a good test coverage, which is not a good indicator, [as this anecdote shows](https://dev.to/conectionist/why-code-coverage-is-not-a-reliable-metric -327l).
EOS is a new and promising blockchain implementation, which uses the Delegate Proof-of-Stake (DPoS) consensus algorithm. It also uses WASM as language to write smart contracts. On the negative side, the lack of adequate analysis on DPoS ([only one explanation exists](https://steemit.com/dpos/@dantheman/dpos-consensus-algorithm-this -missing-white-paper)) suggests careful evaluation of this technology in a real world. Mathematical proof of DPoS would be needed before medical data is injected into EOS. Cardano claims to have such mathematical proof. As an example, recently [De Angelis et al.] proved that the the Proof-of-Authority protocol for permissioned blockchain deployed over WANs experimenting Byzantine nodes, does not provide adequate consistency guarantees for scenarios where data integrity is essential. To my best knowledge no formal proof on DPoS has been done yet.
Again on the performance: the time of doctor is really precious. Time left waiting for a transaction to be processed in the blockchain is time left to the patient treatment: doctors can't simply wait minutes for a HL7 ADT to be processed by the blockchain. We cannot have blockchain stopping healthcare practicionners from admitting a patient.
Some DLT projects utilise pointers to data stored in a off-chain infrastructure. In particular, there are some using FHIR resources identifiers in the blockchain to guarantee a property (e.g., access control, patient-centric access to EHR, or data integrity). I don’t see blockchain acting as a market disruptor, but, in contrast, I see blockchain makes these projects more complicated, for two reasons:
-
If the blockchain deployment is public, and the blockchain uses code "written in stone", then the audit process is not sufficient to keep data secure forever. If the deployment is private, many regulations require the blockchain nodes that act as data controller to be operated under ISO 27002. Keeping many nodes utilising such operating model may be really expensive for hospitals, effectively opening an excellent marketing opportunity for Blockchain-as-a-Service.
-
The benefit of decentralisation is not entirely clear, since a centralised off-chain storage is anyway required (e.g., within a hospital information system).
The second point may have a corollary in the sense that if the goal is to achieve data integrity, and the blockchain implementation used is inefficient, an application including a database with properly signed data (e.g., using any aDES) is more suitable in terms of performance (although I don’t have done any tests).
Other DLT initiatives propose visionary technologies and appealing solutions. However, as we already saw with the EIF story, homogeneity conflicts with interoperability, and lets adapters proliferate to accomodate with yet-another technology.
Healthcare can definitely exploit the DLTs for instance in patient matching, and resource consumption rewards (e.g., paying to access the IT resource).
Patient matching involves the typical case when a patient, or even a doctor, has to be identified and authenticated. There are interesting ideas such as the concept of self-sovereign identities, clinical research, etc. [More information can be found here](https://healthcaresecprivacy.blogspot.com/2017/03/healthcare-blockc hain-use.html).
We see that a product with interfaces and algorithms supported by only one single vendor or organisation cannot be the ideal solution, since it goes against the concepts of the continuum (the software asset which survives to its creator), and produces vendor lock-in, elevating the risks of project failures and, most important, jeopardising patient safety. Also, storing data (even encrypted) in the blockchain is also a weak idea due to performance and security issues.
#Special Thanks
Special thanks to my colleagues and to the FLUG for their help.
#References
[Bass et al] L. Bass, P. Clements, R. Kazman, Software Architecture in Practice, Third Edition, Addison-Wesley 2013
[Meyer] B. Meyer, Agile! The Good, the Hype and the Ugly, Springer 2014
[Babar et al.] M. Babar, A. W. Brown, I. Mistrik, Agile Software Architecture: Aligning Agile Processes and Software Architectures, Morgan Kaufmann Publishers Inc. San Francisco, CA, USA 2013
[Wattenhofer] R. Wattenhofer, The science of the blockchain, Inverted Forest Publishing, 2016
[De Angelis et al.] De Angelis, Stefano & Aniello, Leonardo & Baldoni, Roberto & Lombardi, Federico & Margheri, Andrea & Sassone, V., PBFT vs proof-of-authority: applying the CAP theorem to permissioned blockchain.